2022 WORLD HEPATITIS DAY: Bringing hepatitis care closer to the primary health facilities and communities.

According to World Health Organization (WHO), every 30 seconds someone loses their life to Hepatitis B or C and the world is currently facing a new outbreak of unexplained acute hepatitis infections affecting children. WHO, together with scientists and policymakers in affected countries, are working to understand the cause of this infection that does not appear to belong to any of the known 5 types of hepatitis viruses: A,B,C,D, and E.
WHO maintains that this new outbreak brings focus on thousands of acute viral hepatitis infections that occur among children, adolescents and adults every year. Most acute hepatitis infections cause mild disease and even go undetected. But in some cases, they can lead to complications and be fatal. In 2019 alone, an estimated 78 000 deaths occurred worldwide due to complications of acute hepatitis A to E infections.
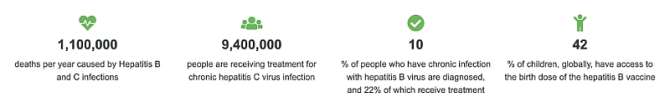
Global efforts prioritize the elimination of the hepatitis infections B, C and D infections. Unlike acute viral hepatitis, these 3 infections cause chronic hepatitis that lasts for several decades and culminate in over 1 million deaths per year from cirrhosis and liver cancer. These 3 types of chronic hepatitis infections are responsible for over 95% of hepatitis deaths. While we have the guidance and tools to diagnose, treat, and prevent chronic viral hepatitis, these services are often out of reach of communities and are sometimes only available at centralized/specialized hospitals.
The main aim of July 28, World Hepatitis Day, is to sensitize and encourage people on how to prevent, diagnose, and treat viral hepatitis infections.
It pains me when patients who received blood transfusion in the past later come down with hepatitis B or C infection and the cause is traceable to no other source except the past blood transfusion.
In view of this, our hospitals should upgrade to the use of Polymerase Chain Reaction (PCR) in screening blood samples ( especially those units of blood from donors with questionable lifestyles) .This is because the current tests used in detecting the viral infections in many hospitals in developing countries are targeted at detecting the antigen or antibody to the infecting viral particles in the serum hence it takes some time ( the incubation period etc ) before the current tests in many developing countries can detect the antigen/antibody in a newly infected individual .PCR can detect the infection at each stage of the disease .
We cannot forget in a hurry the 2006 incident at Lagos University Teaching Hospital (LUTH) where baby Oyinkansola Eniola was transfused with a HIV positive blood in a tertiary hospital where the highest form of medical treatment was expected in line with international best practices . It is a crime and unethical to transfuse a unit of blood without first screening it for HIV 1 & 2, Hepatitis B and C and VDRL among other preliminary tests.
Was the blood screened before the transfusion? Believe you me ,the answer will be in the affirmative ,then why didn't the screening pick up the HIV in the donor's blood? The Window period of HIV infection cannot easily be ruled out at the time of screening that blood hence screening with PCR remains the only trusted test at all stages of the infection .If that was possible with HIV, it is still possible with some of the viral hepatitis, especially hepatitis B and C .
THEME FOR 2022 CELEBRATION : There are two themes for this year’s World Hepatitis day.
WHO is highlighting the need for bringing hepatitis care closer to the primary health facilities and communities so that people have better access to treatment and care, no matter what type of hepatitis they may have.
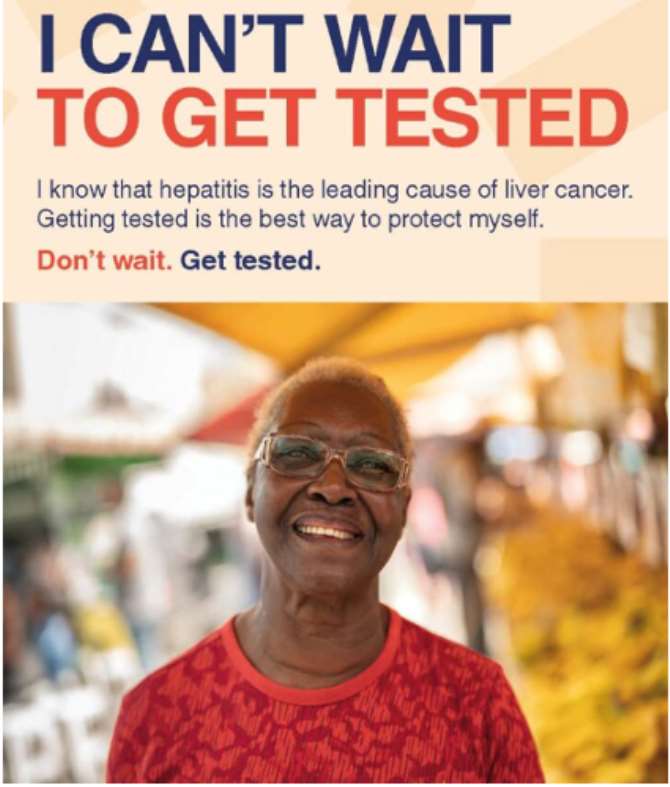
Also, https://www.worldhepatitisday.org/ chooses her theme for this year as: I can’t wait because of the following reasons :
- People living with viral hepatitis unaware can’t wait for testing
- People living with hepatitis can’t wait for life saving treatments
- Expectant mothers can’t wait for hepatitis screening and treatment
- Newborn babies can’t wait for birth dose vaccination
- People affected by hepatitis can’t wait to end stigma and discrimination
- Community organisations can’t wait for greater investment
- Decision makers can’t wait and must act now to make hepatitis elimination a reality through political will and funding.
I can’t wait
‘I can’t wait’ is the new campaign theme to launch World Hepatitis Day 2022. It will highlight the need to accelerate the fight against viral hepatitis and the importance of testing and treatment for the real people who need it. The campaign will amplify the voices of people affected by viral hepatitis calling for immediate action and the end of stigma and discrimination.
BRIEF HISTORY
Initially, the World Hepatitis Day was celebrated on May 19th of each year but in 2010 the World Health Assembly changed the date to July 28th in honour of the birthday of the noble laureate Professor Baruch Samuel Blumberg, who discovered Hepatitis B.
INTRODUCTION:
Below is the 2022 Message From the WHO Regional Director for Africa, Dr Matshidiso Moeti
The world marks World Hepatitis Day on 28 July every year, to raise awareness of this “silent killer” which is responsible for the deaths of about 125 000 people in Africa every year, despite the availability of treatment.
This year’s theme, “Bringing hepatitis care closer to you”, aims to highlight the need to bring hepatitis care closer to primary health care facilities, and so communities, to ensure better access to treatment and care.
More than 90 million people are living with hepatitis in Africa, accounting for 26% of the global total. But because the disease goes mostly undetected due to an absence of symptoms until it is too late for treatment, preventable loss of life is the tragic result.
Today, WHO in the African Region launches the 2021 scorecard for hepatitis, with blood tests revealing high prevalence of Hepatitis B in more than 8% of the total populations of 19 countries. For Hepatitis C, prevalence in 18 countries is more than 1%.
Transmission of Hepatitis B from mother-to-child also remains high, with prevalence of 2.5% among children younger than five in the Region. Only 14 African Region countries have managed to reduce that number to the 1% milestone, which has been achieved by all other WHO Regions.
The 2021 Global Hepatitis Report reminded us that only 2% of people living with Hepatitis B in Africa know their status, and that less than 1% are receiving treatment. For Hepatitis C, only 5% of patients know their status, with an alarming 0% treatment rate.
In addition, only 6% of babies have received the Hepatitis B birth-dose vaccine that prevents transmission of the virus from their mothers. This is a travesty considering the capacity of this available vaccine to save hundreds of thousands of lives.
The main barriers include that hepatitis services are centralized in cities and major urban areas, being delivered primarily by specialists, along with the high cost of diagnosis and medicines, and an inadequate laboratory platform.
In 2021, WHO in the African Region adopted the 2021-2030 Framework for an Integrated Multisectoral Response to TB, HIV, STIs and Hepatitis in region. The aim is to support milestones that include the introduction of the Hepatitis B birth dose vaccine in 35 Member States, the diagnosis of at least 30% of those with chronic hepatitis infections, and the achievement of 30% of people with Hepatitis B and Hepatitis C on treatment.
To reach these ambitious milestones, countries must advance towards decentralized care. WHO is supporting these efforts with the launch of targeted training materials to capacitate health workers to scale up delivery of simplified Hepatitis B and Hepatitis C services, in line with Universal Health Coverage principles.
The many promising developments in the fight to eliminate hepatitis are reason for hope. The launch of the global strategies on hepatitis in 2016 and 2022, along with increased advocacy and political will, are beginning to translate into action.
Hepatitis medications have, for example, become much more affordable, with prices now as low as US$60 per patient for a 12-week course of Hepatitis C treatment. In Rwanda, more than 50 000 patients had received treatment by the end of last year, and countries including Benin, Burkina Faso, Mozambique and Uganda are mobilizing domestic resources to implement hepatitis programmes.
On World Hepatitis Day this year, I call on all African governments to commit to decentralizing care to primary health level, to reach everyone, no matter where they live, and to prioritize funding to address this preventable health threat.
I encourage our countries to capacitate health systems to screen blood donations for hepatitis, and to ensure once-only use of syringes, and their safe disposal. These are important contributors to hepatitis transmission.
Finally, I appeal to people across Africa to seek testing and treatment for hepatitis. We need to take collective responsibility for eliminating this disease by 2030.
WHO believes that the number of deaths due to HIV/AIDS has really changed and expanded access to antiretroviral therapy (ART) and a declining incidence of HIV infections have led to a steep fall globally in the number of adults and children dying from HIV-related causes.
World Hepatitis Alliance (WHA) maintains that globally there are more than 290 million people living with viral hepatitis unaware and without finding the undiagnosed and linking them to care, millions will continue to suffer, and lives will be lost. This is why the theme recognized by WHA for this year’s celebration is Finding the missing millions.
Coming to data available in Nigeria, Dr Chukwuma Anyaike,a Community Health physician , few years ago argued that about 20 million Nigerians are infected with Hepatitis B and C .The said physician who was then the Head, Prevention, Department of Public Health at the Federal Ministry of Health stated this at a one-day stakeholders’ advocacy workshop on Viral Hepatitis awareness organised by the Yakubu Gowon Foundation in Abuja.He further pointed out that ,''Viral Hepatitis is a very big public health issue in Nigeria. By the work Federal Ministry of Health has done, we have 20 million Nigerians living with Hepatitis B and C and they are at the risk of developing cirrhosis of the liver and cancer of the liver. Most importantly, these ones are living in the communities and they are not aware of it and in the same process, they are transferring the infection to other people in the community.”
In the occasion, it was further revealed that approximately 20 million of Nigeria’s 170 million population that are infected by the virus, 25 percent of them go on to develop chronic liver disease and between 500,000 to 700,000 result in deaths annually.
From the survey (2000-2013), Kano had the highest number of people infected with the B variant of the virus while Kwara state had the highest number of people with Hepatitis C.
However , Nigeria HIV/AIDS Indicator and Impact Survey(NAIIS) report currently shows that Nigeria, with an estimated population of 190 million people, has a Hepatitis B prevalence of 8.1% and Hepatitis C at 1.1%
DEFINITION AND CLASSIFICATION:
Hepatitis is a health condition characterized by the presence of inflammatory cells in the tissues of the liver.It can be self-limiting(healing on its own) or can simply progress to fibrosis(scarring),Cirrhosis, liver failure or liver cancer. Hepatitis can be acute when it lasts for less than six months or chronic when it lasts for more than six months.
Viral hepatitis is mainly classified into five groups: Hepatitis A, B, C, D and E. There are other classifications of hepatitis such as autoimmune, alcoholic hepatitis etc., but the main aim of the World Hepatitis Day is to sensitize and encourage people on how to prevent, diagnose and treat these five VIRAL hepatitis infections.
Hepatitis A:
Caused by Hepatitis A virus and it occurs when an uninfected person ingests food or water contaminated with the faeces of an infected person. It can also be contracted through close physical contact with an infectious person, although casual contact among people does not spread the virus. There are about 1.4 million cases each year worldwide. Unlike Hepatitis B & C, it does not run a chronic course but can lead to debilitating symptoms and fulminant hepatitis(acute liver failure), which has a very high mortality rate.
WHO maintains that that :
Hepatitis A is a viral liver disease that can cause mild to severe illness.
- The hepatitis A virus (HAV) is transmitted through ingestion of contaminated food and water or through direct contact with an infectious person.
- Almost everyone recovers fully from hepatitis A with a lifelong immunity. However, a very small proportion of people infected with hepatitis A could die from fulminant hepatitis.
- WHO estimates that hepatitis A caused approximately 7 134 deaths in 2016 (accounting for 0.5% of the mortality due to viral hepatitis).
- The risk of hepatitis A infection is associated with a lack of safe water, and poor sanitation and hygiene (such as dirty hands).
- In countries where the risk of infection from food or water is low, there are outbreaks among men who have sex with men (MSM) and persons who inject drugs (PWIDs).
- Epidemics can be prolonged and cause substantial economic loss.
- A safe and effective vaccine is available to prevent hepatitis A.
- Safe water supply, food safety, improved sanitation, hand washing and the hepatitis A vaccine are the most effective ways to combat the disease. Persons at high risk, such as travelers to countries with high levels of infection, MSM and PWIDs can get vaccinated.
Hepatitis B:
It is a potentially life threatening disease of the liver caused by Hepatitis B virus and it is contracted by contact with the blood or body fluids of an infected person. It is commonly spread from mother to child at birth,or from person to person in early childhood. In the rural settings, it can be contracted by sexual transmission (when no barrier protective measure is used) and the use of contaminated sharp objects like needles, razor blades etc., and inadequately sterilized hospital equipment. It runs both acute and chronic courses and about 240 million individuals globally have chronic Hepatitis B infection whereas in each year, about 780,000 people die globally from acute and chronic Hepatitis B infections. It is an important occupational hazards for health care professionals, members of the Federal Road Safety Corps,commercial sex workers,long distance drivers etc.
WHO still believes that : Hepatitis B is a viral infection that attacks the liver and can cause both acute and chronic disease.
- The virus is most commonly transmitted from mother to child during birth and delivery, as well as through contact with blood or other body fluids, including sex with an infected partner, injection-drug use that involves sharing needles, syringes, or drug-preparation equipment and needle sticks or exposures to sharp instruments.
- WHO estimates that in 2015, 257 million people were living with chronic hepatitis B infection (defined as hepatitis B surface antigen positive).
- In 2015, hepatitis B resulted in an estimated 887 000 deaths, mostly from cirrhosis and hepatocellular carcinoma (i.e. primary liver cancer).
- As of 2016, 27 million people (10.5% of all people estimated to be living with hepatitis B) were aware of their infection, while 4.5 million (16.7%) of the people diagnosed were on treatment. According to latest WHO estimates, the proportion of children under five years of age chronically infected with HBV dropped to just under 1% in 2019 down from around 5% in the pre-vaccine era ranging from the 1980s to the early 2000s.
- Hepatitis B can be prevented by vaccines that are safe, available and effective.
Hepatitis C:
Caused by Hepatitis C virus and it is contracted the same way Hepatitis B infection is contracted through unsafe injection practices;inadequate sterilization of medical equipment in healthcare settings;and unscreened blood and blood products. Like Hepatitis B,it runs both acute and chronic courses but it has more propensity of running chronic course than Hepatitis B.A significant number of the chronic carriers of the disease will come down with Cirrhosis or Liver cancer. It is estimated globally that about 130-150 million people are chronic carriers of the infection while about 350,000-500,000 people die annually from Hepatitis C related infections.
WHO maintains that : Hepatitis C is a liver disease caused by the hepatitis C virus (HCV): the virus can cause both acute and chronic hepatitis, ranging in severity from a mild illness lasting a few weeks to a serious, lifelong illness.
- Hepatitis C is a major cause of liver cancer.
- The hepatitis C virus is a bloodborne virus: the most common modes of infection are through exposure to small quantities of blood. This may happen through injection drug use, unsafe injection practices, unsafe health care, transfusion of unscreened blood and blood products, and sexual practices that lead to exposure to blood.
- Globally, an estimated 71 million people have chronic hepatitis C virus infection.
- A significant number of those who are chronically infected will develop cirrhosis or liver cancer.
- WHO estimated that in 2016, approximately 399 000 people died from hepatitis C, mostly from cirrhosis and hepatocellular carcinoma (primary liver cancer).
- Antiviral medicines can cure more than 95% of persons with hepatitis C infection, thereby reducing the risk of death from cirrhosis and liver cancer, but access to diagnosis and treatment is low.
- There is currently no effective vaccine against hepatitis C; however, research in this area is ongoing.
Hepatitis D:
Caused by Hepatitis D virus, which is called an incomplete virus or subviral satellite because it can propagate only in the presence of Hepatitis B virus,hence the transmission of Hepatitis D can only occur either via simultaneous infection with hepatitis B virus(co-infection) or superimposed on chronic Hepatitis B carrier state (superinfection). Regrettably, in combination with Hepatitis B virus, Hepatitis D infection has the highest mortality rate of all the Hepatitis infections.
WHO is of the opinion that : Hepatitis D virus (HDV) is a virus that requires hepatitis B virus (HBV) for its replication. HDV infection occurs only simultaneously or as super-infection with HBV.
- The virus is most commonly transmitted from mother to child during birth and delivery, as well as through contact with blood or other body fluids, including sex with an infected partner, injection-drug use that involves sharing needles, syringes, or drug-preparation equipment and needle sticks or exposures to sharp instruments.
- Vertical transmission from mother to child is rare.
- Hepatitis D virus (HDV) affects globally nearly 5% of people who have a chronic infection with hepatitis B virus (HBV).
- Several geographical hotspots of high prevalence of HDV infection exist, including Mongolia, the Republic of Moldova, and countries in Western and Middle Africa.
- Populations that are more likely to have HBV and HDV co-infection include people who inject drugs, indigenous populations and recipients of hemodialysis.
- Worldwide, the overall number of HDV infection has decreased since 1980s. This trend is mainly due to a successful global HBV vaccination programme.
- HDV-HBV co-infection is considered the most severe form of chronic viral hepatitis due to more rapid progression towards liver-related death and hepatocellular carcinoma.
- Currently, treatment success rates are generally low.
- Hepatitis D infection can be prevented by hepatitis B immunization.
Hepatitis E:
Caused by Hepatitis E virus and mainly transmitted through contaminated drinking water. Less commonly,it can also be transmitted by transfusion of infected blood products and vertical transmission from a pregnant woman to her fetus. It is self-limiting,resolving within four to six weeks,though it may at times run a fulminant course(acute liver failure) leading to death. Globally, there are approximately 20 million incidents of Hepatitis E infections every year; three million acute cases; 56,600 hepatitis E-related deaths. Hepatitis E can also induce a mortality of about 20% among pregnant women in their third trimester.
Finally , WHO opines that Hepatitis E is a liver disease caused by infection with a virus known as hepatitis E virus (HEV).
- Every year, there are an estimated 20 million HEV infections worldwide, leading to an estimated 3.3 million symptomatic cases of hepatitis E (1).
- WHO estimates that hepatitis E caused approximately 44 000 deaths in 2015 (accounting for 3.3% of the mortality due to viral hepatitis).
- The virus is transmitted via the fecal-oral route, principally via contaminated water.
- Hepatitis E is found worldwide, but the disease is most common in East and South Asia.
- A vaccine to prevent hepatitis E virus infection has been developed and is licensed in China, but is not yet available elsewhere.
CLINICAL FEATURES:
The viral hepatitis infections have almost common features which can be asymptomatic (no symptoms) but often lead to jaundice, loss of appetite, and malaise. As noted earlier on, some of them can run either acute or chronic courses.
The acute features:
In children, the features are usually asymptomatic while in older individuals, there may be nonspecific flu-like symptoms,common to almost all acute viral infections which include: malaise; muscle and joint aches; fever; nausea or vomiting; diarrhoea; headache. The more specific acute features include: loss of appetite; aversion to smoking (among smokers); dark urine; yellowing of the eyes and the skin; enlargement of the liver; enlarged lymph nodes in about 5%; enlargement of the spleen.
Meanwhile, a small proportion of the people with acute infections can develop liver failure with associated hepatic encephalopathy (confusion and coma due to inability of the liver to perform its functions); peripheral edema and bleeding.
The chronic features: Although they may present with malaise; tiredness; weakness; jaundice, individuals with chronic infections usually run asymptomatic courses until complicated with cirrhosis, liver cancer, and liver failure.
PREVENTION:
WHO maintains that Hepatitis B is a viral infection that attacks the liver. Hepatitis B vaccine for infants had been introduced nationwide in 190 Member States by the end of 2021. Global coverage with 3 doses of hepatitis B vaccine is estimated at 80%. In addition, 111 Member States introduced nationwide 1 dose of hepatitis B vaccine to newborns within the first 24 hours of life. Global coverage is 42% and is as high as 78% in the WHO Western Pacific Region, while it is only estimated to be at 17% in the WHO African Region.
This is the theme for this year's World Hepatitis day. It is generally believed that ,'prevention is better than cure.' The transmission of the virus can be prevented through better awareness and services that improve vaccinations ,blood and injection safety,and reduce harm. This annual campaign aims not only to raise awareness among the general public and infected patients,but also to urgently promote improved access to hepatitis services ,particularly prevention interventions by policymakers.
WHO aims to achieve hepatitis elimination by 2030. To get there, WHO calls on countries to achieve specific targets:
- Reduce new infections of hepatitis B and C by 90%;
- Reduce hepatitis related deaths from liver cirrhosis and cancer by 65%;
- Ensure that at least 90% of people with hepatitis B and C virus are diagnosed; and
- At least 80% of those eligible receive appropriate treatment.
Hepatitis A can be prevented by adequate supplies of safe drinking water; proper disposal of sewage within the communities; personal hygiene such as regular hand washing with safe water and soap; getting immunized with Hepatitis A vaccine.
Hepatitis B can be prevented by quality-assured screening of all donated blood and blood components used for transfusion;safe injection practices; safe sex practices,including minimizing the number of partners and using barrier protective measures (condom). Moreover, Hepatitis B vaccine is the mainstay of prevention, no wonder it is part of our National Programme On Immunization. However, adults who were not immunized at childhood and who are among the high risk groups should meet their doctors to ascertain if they are eligible for the vaccination.
Hepatitis C and D infections have almost the same preventive measures as Hepatitis B except that Hepatitis C vaccine is currently unavailable globally though research is still ongoing.
Hepatitis E can be prevented by maintaining quality standards for public water suppliers;establishing proper disposal systems to eliminate sanitary wastes; maintaining hygienic practices such as hand washing with safe water, particularly before handling food; avoiding water/or ice of unknown purity; adhering to WHO safe food practices. Hepatitis E vaccine is still not available in the global market, though it has been produced and licensed in China.
DIAGNOSES AND TREATMENTS:
Consult the nearest medical doctor who is professionally trained to make the diagnosis from clinical history,physical examination and interpretation of laboratory investigation results . The doctor knows when to refer you to a specialist (Gastroenterologist) who is also professionally trained to use simple non-invasive tests to assess the stage of the disease,prioritise treatment for those at advanced stages of the disease,make use of safe and highly effective medications in the treatment and to further monitor the progress of the treatment or disease using simple tests. The managing medical doctor can as well advise you on the need to get vaccinated especially if you tested negative to the virus(s) in order to prevent occupational hazards for those whose occupations involve handling of human blood and other bodily fluids.
In view of the above, our government should map out comprehensive national guideline to tackle this silent killer called viral hepatitis especially in our rural communities since many women get to know their statuses during antenatal period where the hospitals make it compulsory that all pregnant women must be tested for HIV 1 & 2, Hepatitis B and C , VDRL( for syphilis) among other relevant tests. Hepatitis B can easily be transmitted from mother to the baby during pregnancy or at birth.
Dr Paul John,Port Harcourt, 08083658038, [email protected]